Living with chronic back pain can feel like carrying an invisible weight every day. It affects how you move, work, and sleep — sometimes even how you think.
Thank you for reading this post, don't forget to subscribe!In most cases, chronic back pain can be effectively managed without going under the knife.
How to Manage Chronic Back Pain Without Surgery
From physical therapy to lifestyle changes, there are proven, evidence-based treatments that can reduce pain, restore mobility, and improve your quality of life.
This comprehensive guide breaks down everything you need to know about non-surgical back pain management, including physical therapy techniques, medications, mind-body strategies, and when to consider specialist care.
Understanding Chronic Back Pain: Causes and Scope
Chronic back pain is defined as pain lasting 12 weeks or longer, even after the initial injury or underlying cause has been treated. It can stem from mechanical issues in the spine, inflammation, or even nerve compression — and it often persists due to a combination of physical and psychological factors.
According to the CDC, back pain affects nearly 1 in 4 adults, making it one of the most common reasons for missed work and medical visits. The key to effective management lies in understanding what’s driving the pain and targeting the root cause with the right non-surgical treatments.
Common Causes of Non-Surgical Chronic Back Pain
Not all chronic back pain requires surgical intervention. In fact, most cases can be managed conservatively. Below are some of the most common non-surgical causes:
1. Herniated Discs
A herniated or “slipped” disc occurs when the soft cushioning between spinal vertebrae bulges or ruptures, pressing on nearby nerves. This can cause lower back pain, sciatica, and leg numbness. Physical therapy and core strengthening are usually first-line treatments before surgery is ever considered.
2. Degenerative Disc Disease
With age, spinal discs lose hydration and elasticity, leading to pain and stiffness. This is common in older adults and is often managed with exercise therapy, anti-inflammatory medications, and ergonomic adjustments rather than surgery.
3. Spinal Stenosis
This disorder is characterized by a narrowing of the spinal canal, which compresses nerves and results in lower back and leg pain or tingling. Regular stretching, targeted exercises, and injections may relieve symptoms significantly.
4. Muscle Strain or Ligament Sprain
The most common cause of back pain is simple overuse, lifting injuries, or poor posture. These strains can become chronic if not rehabilitated properly. Postural correction, stretching, and strengthening exercises are the cornerstones of recovery.
Physical Therapy (PT): The Foundation of Non-Surgical Back Pain Relief
Physical therapy is the best option for treating chronic back pain without surgery. In addition to relieving pain, a well-designed physical therapy program restores strength, flexibility, and movement patterns to stop recurrences.
Physical therapists design personalized treatment plans that cater to your unique functional goals, pain tolerance, and specific diagnosis.
The regimens often include important elements like core stability exercises that strengthen the body’s foundation, flexibility training to improve range of motion, posture correction techniques that promote proper alignment, and manual therapy for pain relief.
Each component works harmoniously to support your journey toward recovery and improved physical well-being.
Core Strengthening for Spinal Stability
The core muscles — including your abdominals, obliques, and lower back — act as a natural brace for your spine. Chronic pain and instability can result from weak core muscles.
A PT-guided core program may include:
- Pelvic tilts and bridges for lower spine support
- Planks and bird dogs for endurance and balance
- Swiss ball exercises to activate deep stabilizers
Building a strong core not only reduces pain but also prevents reinjury by distributing stress more evenly through your body.
Flexibility Training to Increase Range of Motion
Tight muscles — especially in the hamstrings, hips, and lower back — can worsen pain and limit movement. Flexibility exercises help:
- Improve circulation
- Reduce stiffness
- Enhance range of motion.
Popular PT-recommended stretches include:
- Knee-to-chest stretches
- Cat-cow and child’s pose for spinal mobility
- Seated hamstring stretches for lower back relief.
Flexibility training works best when paired with strength exercises for a balanced program.
Postural Exercises for Long-Term Pain Reduction
Poor posture contributes to chronic tension and misalignment of the spine. Postural retraining teaches you to maintain proper spinal curves during daily activities.
Therapists often recommend:
- Wall angels to open the chest.
- Chin tucks to strengthen neck alignment.
- Scapular retraction exercises to correct rounded shoulders
Over time, these exercises reduce stress on spinal joints and promote natural alignment, easing chronic discomfort.
Key Benefits of a Consistent Physical Therapy Routine
Consistency is everything in physical therapy. Regular sessions deliver:
- Improved mobility and flexibility
- Reduced pain intensity
- Better posture and muscle balance
- Increased confidence in movement
- Prevention of future flare-ups
Many patients find that after 6–8 weeks of steady PT, their reliance on medication drops significantly — a major milestone in non-surgical pain control.
Medications & Injections for Chronic Back Pain Management
Medication can play an important supportive role, especially during flare-ups. The goal is to reduce inflammation and nerve irritation while maintaining activity levels.
Over-the-Counter (OTC) Anti-Inflammatory Medications
For mild to moderate pain, NSAIDs (non-steroidal anti-inflammatory drugs) like ibuprofen and naproxen are often the first line of defense. These medications:
- Reduce swelling around irritated nerves.
- Provide temporary relief for daily function.
- Work best when paired with physical therapy.
It’s important to use them as directed to avoid side effects such as stomach irritation or increased blood pressure.
When to Use Prescription-Strength NSAIDs (Risks & Monitoring)
If OTC medications aren’t effective, doctors may prescribe stronger NSAIDs or muscle relaxants. These require close monitoring due to potential side effects, including:
- Gastrointestinal bleeding
- Kidney strain
- Heart risks with long-term use.
Prescription medications should be seen as short-term aids, not long-term solutions.
Targeted Injection Therapies (ESI and Facet Joint Injections)
For persistent inflammation, injection therapies can provide targeted relief:
- Epidural Steroid Injections (ESI) reduce nerve root inflammation from herniated discs.
- Facet Joint Injections help relieve localized arthritic or joint-related pain.
Usually carried out under imaging supervision, these operations can reduce discomfort for weeks or months, enabling patients to complete their rehabilitation and remain active.
Mind-Body Techniques: Addressing the Psychological Side of Pain
Chronic pain doesn’t just affect the body — it alters how the brain processes discomfort. Over time, pain pathways can become hypersensitive.
This is where mind-body techniques step in, helping reframe the experience of pain.
Cognitive Behavioral Therapy (CBT) for Pain Reframing

CBT helps patients change negative thought patterns that intensify pain perception. A therapist works with you to:
- Recognize unhelpful beliefs (“I can’t move because it’ll hurt”)
- Replace them with adaptive coping strategies.
- Build mental resilience and stress tolerance.
Research shows CBT can reduce pain intensity and disability, often matching or exceeding the effects of medication in long-term studies.
Mindfulness Meditation to Reduce Emotional Distress
Mindfulness helps you stay present with sensations without reacting emotionally. Regular practice lowers stress hormones and reduces the brain’s pain response.
Try:
- 10 minutes of guided breathing or body scanning daily
- Meditation apps or classes that focus on chronic pain relief
- Combining mindfulness with stretching or yoga
Patients often report that mindfulness helps them accept pain without fear, breaking the pain-tension cycle.
Hands-On Treatment: Chiropractic Care and Massage Therapy
Manual therapy techniques can complement medical and physical therapy treatments by targeting muscle tension, joint misalignment, and circulation.
Spinal Adjustments with Chiropractic Care
Chiropractors use controlled adjustments to restore motion to stiff spinal joints. This can relieve pressure on nerves, improve posture, and enhance spinal mobility. Chiropractic therapy is not always appropriate, but it can be helpful when:
- Pain stems from joint restriction.
- There’s no spinal instability or fracture.
- It’s combined with exercise therapy.
Always ensure adjustments are performed by a licensed chiropractor familiar with your condition.
Massage Therapy for Muscle Relaxation and Blood Flow
Chronic back pain often leads to muscle guarding — tightness that limits motion. Therapeutic massage promotes:
- Muscle relaxation
- Improved blood flow and tissue healing
- Endorphin release for natural pain relief
Popular techniques include deep tissue, myofascial release, and trigger point therapy. Weekly or biweekly sessions are beneficial for many people.
Acupuncture: Stimulating Natural Pain Relief (Endorphins)
In order to activate the nerve system, acupuncture, which has its roots in traditional Chinese medicine, uses tiny needles inserted at predetermined sites. Studies show it can:
- Increase endorphin production
- Improve circulation
- Decrease chronic pain levels.
It’s a safe, low-risk option when performed by a certified practitioner, and it is often used alongside Western therapies for a holistic approach.
Essential Lifestyle Changes for Long-Term Back Health
Even the best therapy won’t last if daily habits continue to strain your back. Sustainable relief depends on lifestyle alignment — strengthening your back through smart, consistent choices.
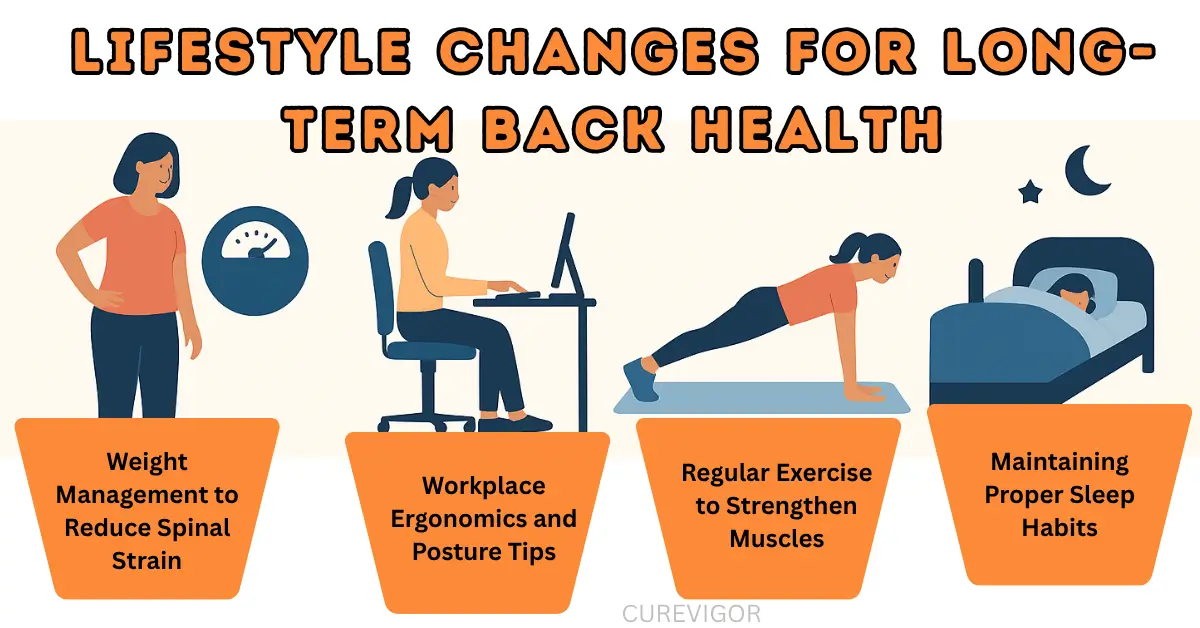
Weight Management to Reduce Spinal Strain
Being overweight puts more strain on the joints and spinal discs, particularly in the area surrounding the abdomen. Losing even 10–15 pounds can significantly decrease pain. A balanced approach includes:
- Whole foods rich in anti-inflammatory nutrients (omega-3s, leafy greens, lean proteins)
- Regular low-impact exercise (walking, swimming, or cycling)
- Proper hydration and sleep for muscle recovery
Maintaining a healthy weight supports spinal alignment and reduces the risk of flare-ups.
Workplace Ergonomics and Posture Tips
Many cases of back pain trace back to poor workstation setup or prolonged sitting. Fixing ergonomics can make a huge difference:
- Use an adjustable chair with lumbar support.
- Keep your screen at eye level.
- Stand and stretch every 30–45 minutes.
- Consider a sit-stand desk to vary posture.
At home, avoid slouching on soft couches for long hours — sit upright with your back supported and feet flat on the floor.
Regular Exercise to Strengthen Muscles
A sedentary lifestyle weakens the muscles that support your spine, increasing the risk of chronic pain. Regular, low-impact exercise strengthens your back, core, and surrounding muscles, improving stability and flexibility. A well-rounded routine includes:
- Strength training for core and lower back support
- Stretching or yoga to maintain mobility
- Low-impact cardio (walking, swimming, cycling) for circulation
Keeping your muscles active protects your spine, improves posture, and helps prevent future pain flare-ups.
Maintaining Proper Sleep Habits
Poor sleep posture can strain spinal alignment and worsen pain over time. Quality rest allows the body to repair muscles and discs affected by daily stress. To support recovery, focus on:
- Using a medium-firm mattress for spinal support
- Sleeping on your side or back with proper pillow placement
- Keeping a consistent sleep schedule for hormone balance
Good sleep hygiene not only reduces inflammation but also enhances your body’s ability to heal, keeping your back healthy and strong.
When to Consult a Specialist: Considering Surgery
Despite best efforts, some cases of chronic back pain may not improve with conservative treatments. Consult a spine specialist or orthopedic surgeon if:
- Pain radiates down the leg and limits walking.
- You feel weak, numb, or lose control over your bowels or bladder.
- Non-surgical treatments fail after several months.
Surgery is typically reserved for specific structural problems (like severe herniated discs or spinal instability). However, many patients find that exploring a multidisciplinary non-surgical program delays or avoids the need for surgery entirely.
Frequently Asked Questions (FAQs) on Non-Surgical Back Pain Relief
Q: How Do I Fix My Back Pain Without Surgery?
Begin with a structured physical therapy program. Combine this with anti-inflammatory medication, posture correction, and light activities such as walking or swimming.
Consider injections, chiropractic adjustments, or acupuncture as part of an all-encompassing therapy approach if the pain persists.
Q: Is Chronic Back Pain Curable or Only Manageable?
Chronic back pain can be a persistent shadow in one’s life, often proving to be manageable rather than completely curable, depending on its underlying cause.
However, many people find that they can live pain-free or with just mild discomfort for years with a careful combination of focused therapy, energizing exercise, and significant lifestyle changes.
This journey towards relief allows them to reclaim their lives, embracing activities they once cherished with renewed vigor and ease.
Q: Is There a Permanent Cure for Lower Back Pain?
For most people, there isn’t a one-time cure — but long-term relief is absolutely possible. A combination of strength training, ergonomic adjustments, and consistent movement can prevent pain from returning.
Q: How Do People Live With Chronic Back Pain?
People manage it through a holistic approach: regular exercise, stretching, therapy, mindfulness, and pacing activities to avoid flare-ups.
Staying active and maintaining social and emotional health are just as important as medical treatment.
Q: Can You Fully Recover from Chronic Pain?
Yes, many do. Recovery doesn’t always mean total elimination of pain — it means regaining control and function. With time and persistence, pain becomes a background sensation instead of the defining feature of your life.
Q: What Do You Do If Back Pain Doesn’t Go Away?
If pain persists beyond three months, it’s time for diagnostic imaging and a specialist consultation. Persistent pain may indicate nerve compression or arthritis that needs targeted treatment like injections or advanced physical therapy.
Conclusion: A Multidisciplinary Approach to Back Pain Management
Managing chronic back pain without surgery requires patience, consistency, and a team approach. No single treatment works for everyone, but when physical therapy, medications, mind-body techniques, and lifestyle changes come together, results can be life-changing.
By understanding the causes, staying active, and embracing a comprehensive non-surgical strategy, you can regain control, restore mobility, and live well again — free from the shadow of chronic pain.
Read more Health & Wellness Tips.
You might like to read:

